Unmasking Necrobiosis Lipoidica: A Window into Non-Diabetic Granulomatous Dermatitis
In a revealing case study, a 43-year-old woman’s long-term skin condition provides insight into necrobiosis lipoidica, a chronic granulomatous dermatitis often associated with diabetes. This case is particularly intriguing as it manifests in a non-diabetic individual, challenging common perceptions and underlining the importance of thorough dermatological assessment irrespective of glycemic status.
Key Points:
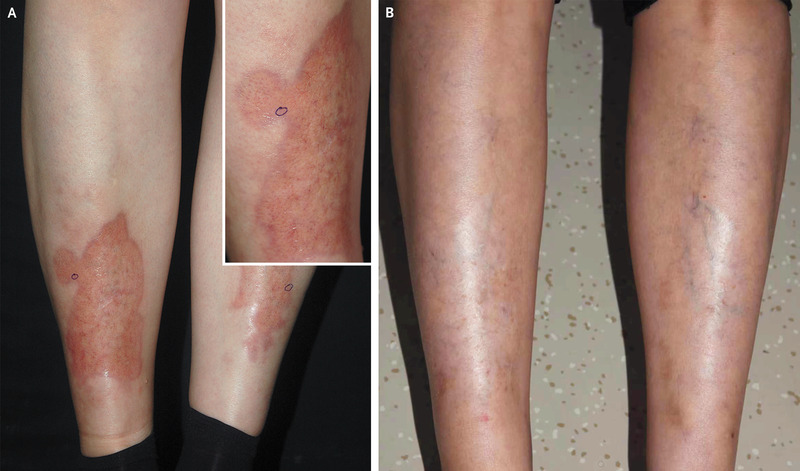
- Patient Profile: 43-year-old woman with an 8-year history of yellow-brown spots on her shins, initially asymptomatic.
- Physical Examination: Presented atrophic yellow-brown plaques with telangiectasias and irregular violaceous borders on both shins.
- Histopathological Findings: Necrobiosis within the dermis, perivascular inflammatory-cell infiltrates, collagen degeneration, consistent with granulomatous dermatitis.
- Diagnosis: Necrobiosis lipoidica, typically associated with diabetes, yet notable in this case for occurring in a non-diabetic patient.
- Treatment and Follow-Up: Initial use of topical glucocorticoids discontinued due to minimal improvement. Remarkable resolution of plaques observed after 13 years without specific treatment.
- Glycemic Status: Normal results on glycemic testing, both initially and at 13-year follow-up, reinforcing the rarity of the condition in non-diabetic individuals.
- Broader Implications: Highlights the necessity for dermatologists to consider necrobiosis lipoidica in non-diabetic patients, expanding the diagnostic scope.

According to the National Center for Biotechnology Information, necrobiosis lipoidica, although closely associated with diabetes, occurs in only 0.3% of diabetic patients. This rarity underscores the importance of considering it in differential diagnoses for similar skin lesions.
More on Skin Conditions/Rash
