A Case Study on Misdiagnosis and Effective Management
In an enlightening case report, a 37-year-old man with epilepsy presented with a severe complication of nasal herpes simplex virus (HSV) infection, initially misdiagnosed as a skin and soft-tissue infection. This case reinforces the diagnostic challenges and emphasizes the importance of a comprehensive approach to patient care, highlighting the broad differential diagnosis and the effective management strategies for HSV infections. The patient’s journey from the onset of symptoms through to recovery provides critical insights into the complexities of diagnosing and treating HSV infections, particularly in non-typical presentations.
Key Points:
- A 37-year-old man experienced significant skin changes on his nose following a scratch, which was exacerbated by trauma during a seizure, leading to a black appearance and swelling of the nose, accompanied by headaches.
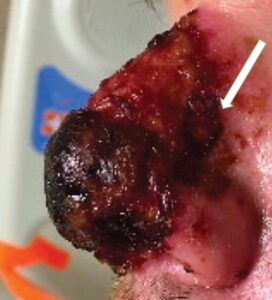
- Initial treatment at another hospital with doxycycline for suspected skin and soft-tissue infection proved inadequate, prompting further evaluation upon presenting to the emergency department where extensive necrosis of the nasal skin was feared.
- Physical examination revealed hemorrhagic crusting, ulceration, and black eschar with peripheral erythema, raising concerns for extensive nasal skin necrosis.
- Laboratory tests showed elevated C-reactive protein levels, but blood cultures and lumbar puncture results were negative, indicating no systemic infection.
- Imaging studies ruled out bony erosion, while nasal endoscopy found healthy nasal mucosa, complicating the diagnosis.
- Biopsy and PCR testing identified HSV-2 as the causative agent, despite the absence of typical systemic symptoms, highlighting the unusual presentation of this case.
- The patient’s treatment regimen included intravenous vancomycin, clindamycin, piperacillin-tazobactam, followed by acyclovir, and eventually oral valacyclovir and amoxicillin-clavulanate, leading to significant improvement.
- Differential diagnosis considered included various infections (eg, HSV-1, Chikungunya virus, invasive fungal infections), inflammatory conditions (eg, granulomatosis with polyangiitis), and neoplasms, demonstrating the need for a broad diagnostic approach.
- The case emphasizes the importance of considering HSV in the differential diagnosis of necrotic nasal lesions, especially with a history of trauma, and the effectiveness of antiviral therapy in management.

According to the World Health Organization, an estimated 3.7 billion people under the age of 50 (67% of the population) have HSV-1 infection globally. This fact underscores the widespread prevalence of herpes simplex virus, though not all infections lead to clinical symptoms.
More on Infectious Diseases
